Attachment Injuries
Now that we have a rudimentary understanding of the necessity for, and basis of attachment behavior, we can begin to discuss attachment injuries and their effects. The term “attachment injury” refers to trauma that occurs within the context of a relationship. In order to understand the impact of relational trauma, consider an analogy from the field of physiology.
Lessons From Physiology
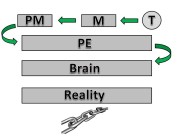
Proprioception is the body’s sense of where it is in space. It is the cumulative interpretation of the body’s various internal and external sensory systems that allow it to have an accurate assessment of the external enivronment. In layman’s terms, it is the body’s sense that allows a person to walk up the stairs or type at a keyboard without the necessity of visual information. When areas of the body are damaged or injured, this vital sensory ability is one of the first casualties. Musculoskeletal injuries result in impaired functioning of this vital sensory feedback system. This results in the increased likelihood of future injury, as the body has a reduced kinesthetic (body movement) awareness of the injured limb or joint.
The parallels between this sensory system and the attachment system are easy to see. Attachment theorists propose that injuries to a person’s relational sensory system increase the chances of future attachment injury as the individual no longer has the wherewithal to make accurate assessments with regard to the safety status of potential attachment figures. In other words, attachment injuries lessen a person’s ability to make accurate assessments of themselves and others, exposing them to the possibility of retraumatization.
Relational Clumsiness
Researchers Laurie Pearlman and Christine Courtois expand on the effects of chronic developmental trauma on interpersonal interaction, stating that relationship problems that arise from attachment injuries “…make it difficult for other to relate to [survivors of complex trauma], in turn, leading to considerable social alienation and isolation and compounding the original effects of the traumatic experiences as individuals are deprived of the very things…that have been found to buffer…those effects”. Pearlman and Courtois go on to describe how individuals with complex trauma histories tend to enter relationships with others who share their traumatic history and who are as equally poorly equipped to manage relationships, thus perpetuating the cycle of relational dysfunction.
Treatment of Complex Trauma Stress
Scientific exploration of these ideas is a relatively new focus in clinical research. Most studies that have been completed seem to focus on the effectiveness of non cognitive-behavior therapy (CBT) approaches to treatment, arguing that CBT minimizes the importance of the relationship between client and counsellor, thus missing the mark with complex trauma cases. These researchers propose that because the relational difficulties aspect of CPTSD opens individuals to an increased chance of retraumatization, the relationship must be the primary focus of treatment.
Once again, the parallel between the treatment for musculoskeletal injuries that result in decreased proprioception is an appropriate analogy. Experts recommend that in the treatment of muscle or tissue injuries, proprioceptive impairments must receive special attention. They point out the necessity of a specific proprioceptive focus in rehabilitation due to the demonstrated link between proprioceptive impairment and re-injury, despite traditional rehabilitation approaches that focus on strengthening joints and the respective supporting muscles. Attachment theorists, such as those cited above, propose that if treatment focuses exclusively, or even mainly, on the “supporting” symptoms, such as re-experiencing, avoidance, and stress tolerance, the client remains a high risk for re-traumatization due to the ineffective relationship filters that the client retains.
A Working Alliance
Before examining the treatment approaches advocated by attachment theorists, a brief review of the impact of the client-therapist relationship on therapeutic outcome is warranted. This relationship (often referred to as the working alliance; WA), has been defined as the agreed-upon tasks and goals, as well as the experience of a personal bond between client and therapist. It has been demonstrated to be the single largest predictor of therapeutic outcome outside of what the client themselves bring to the process(i.e. willingness, symptom severity, etc.). Research has demonstrated that the WA and other interpersonal dimensions of therapy accounted for roughly 30% of the variation in therapeutic outcome.From these results, it has become a widely accepted notion that the WA is a facet of therapy that is deserving of attention. Given the attachment theory reviewed previously, it is easy to see why this construct can be seen as so vital for successful outcome of treatment for CPTSD.
If the working alliance is so important to therapeutic outcome, what then becomes of a client population with whom the inability to form healthy and productive relationships is the primary issue? To be quite frank, these clients are underserved and in many cases, more harm than good is done. When working with people who have complex trauma histories, agencies, institutions, and individual therapists must take the relational difficulties into account. They must recognize that prior to any of the standard therapy tools being employed, the relationship must be the focus of therapy. This does not mean coddling the client out of fear of upsetting the apple cart, but to push the client appropriately and not beyond. Having letters behind your name as a therapist does not automatically instil trust and confidence on the part of the client. In fact, in many cases of CPTSD, it may achieve the opposite. Do not take the client’s trust for granted. It is something that must be worked for and once it is achieved, we must work to maintain it. This is the most fundamental aspect of helping.











































Great site. I’m currently in the early stages of treatment for CPTSD. I’m not a complete disaster, quite functional in fact holding down a good job, and enjoying good friendships (although close intimate relationships are lacking and I can’t say I have much support. Only a couple of friends know about the CPTSD.) It’s tough though. I only truly feel safe amongst people I’ve known for a long time.
Anyways, thank you for the site. It’s informative and helpful.